TSUKUBA FUTURE
#121 Science of the Microorganism Society
Assistant Professor OBANA Nozomu, Institute of Medicine

Bacteria are living organisms that are found in every corner of the earth. They are resilient enough to survive in extreme environments, such as the deep sea, high mountains, and underground settings, as well as in the bodies of animals, including humans, and adapt to diverse environments. One survival strategy that has recently garnered attention is the formation of biofilms or microbial communities. A biofilm is an aggregate of bacteria. Dental plaque, which contributes to tooth decay, is a type of biofilm. Biofilm formation can cause dental caries and periodontal disease. Other common examples of biofilms are the slimy residues found in kitchen sinks, bathtubs, and drains. It is also believed that many bacteria in the human gut exist in biofilms.
Contrary to the common belief that bacteria exist as single-celled organisms, numerous studies have suggested that most microorganisms on earth live in biofilm communities. Current research has shown that bacterial cells within biofilms, even those composed of a single species, share roles. They develop resilience to environmental stresses and antibiotics, similar to the cooperative survival tactics seen in social insects, such as ants and bees.
Interestingly, a research team led by Obana found that Clostridium perfringens, a bacterium responsible for food poisoning and gas gangrene, produces different types of biofilms depending on the surrounding temperature.
Typically, bacteria residing in the human body modulate their activities in response to the body temperature of their host, which is approximately 37°C. However, C. perfringens forms a thick elastic pellicle biofilm at the relatively cooler temperature of approximately 25°C, which is below the average temperature of the human body. Conversely, at approximately 37°C, this bacterium does not form a thick pellicle biofilm but instead develops a different biofilm structure that adheres densely to host cell surfaces. In their research, Obana and his team discovered a gene necessary for C. perfringens to form elastic pellicle biofilms. This gene encodes a protein named BsaA (biofilm self-assembling protein A), which self-polymerizes and creates a highly stable fibrous structure that remains intact even when exposed to surfactants and strong acids.
Interestingly, C. perfringens is a strict anaerobe that dies when exposed to atmospheric oxygen levels. However, when encased in BsaA polymers and the resultant thick pellicle biofilms, these bacteria gain enhanced resistance to both oxygen and antibiotics such as penicillin. The team also observed that within the biofilm, the bacterial cells were divided into BsaA-producing and non-producing cells, indicating division of labor and collective survival within the biofilm.
This study offers insights into how anaerobic gut bacteria such as C. perfringens survive outside their host. Once excreted from the host body, C. perfringens senses temperatures lower than those of the host body and produces BsaA polymers as a protective shield against an oxygen-rich external environment. Simultaneously, non-BsaA-producing cells attach to host cell surfaces. This division of labor serves as a survival strategy for C. perfringens against environmental changes. Further exploration of this survival strategy through biofilm formation could aid in the prevention and treatment of diseases associated with gut bacteria.
Dr. Obana often tells his students, "Don't just say that the experiment failed but think about the reasons for the results. That will lead to discoveries." In the C. perfringens biofilm research, the starting point was an error in setting the incubation temperature.
In March of this year (2023), an international research team headed by Obana reported new findings regarding gut pathogens. Their research focused primarily on a bacterium called Clostridioides difficile, which is resistant to antibiotics and can cause severe diarrheal infections.
Numerous types of bacteria coexist in equilibrium in the human intestine. However, this balance can sometimes get disrupted during antibiotic treatment, leading to abnormal proliferation of antibiotic-resistant bacteria. A significant issue related to this imbalance is the C. diff infection (CDI). The research team analyzed the genome data of various bacteria and discovered that many bacteria, including C. diff, possess the ARE-ABCF gene that imparts antibiotic resistance.
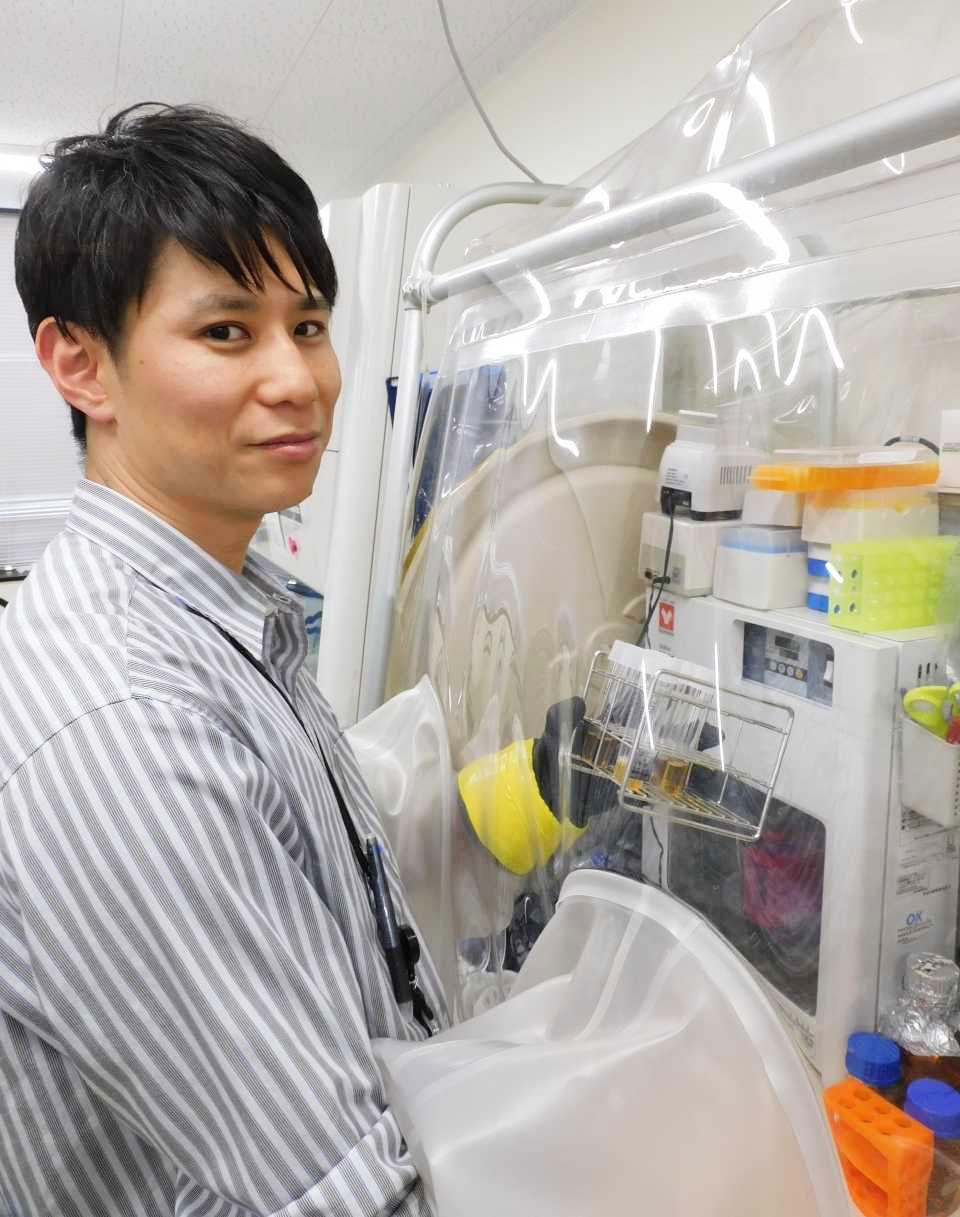
Anaerobic bacteria are cultured in an oxygen-free chamber.
Furthermore, the team demonstrated that the ARE-ABCF gene in C. diff (known as cplR) can provide resistance against the lincosamide and pleuromutilin antibiotics. These antibiotics usually inhibit bacterial growth by attaching to the ribosome, the intracellular protein synthesizer, thus blocking protein synthesis. However, they found that in the case of C. diff, when the antibiotic binds to the ribosome, cplR is expressed in the C. diff cells and dislodges the antibiotics from the ribosome.
The study also revealed that cplR is conserved in C. perfringens and highly pathogenic bacteria, such as Clostridium botulinum. Further elucidation of this resistance factor could contribute to the development of preventive and therapeutic measures for CDI and countermeasures against emerging antibiotic-resistant bacteria.
Since his childhood, Obana has had a keen interest in living organisms, which led him to study at the College of Biological Sciences at the University of Tsukuba. During his graduate studies, he researched the molecular mechanisms that regulate gene expression. After completing his doctoral studies, he joined a laboratory, where he was fascinated upon discovering that microorganisms also form societies, inspiring him to broaden his research. "You can be the first to know something that no one on earth knows. That's what makes research so exciting and fun," he says. His eagerly anticipated future research will explore the relationship between gut bacteria and immunity.
Article by Science Communicator at the Bureau of Public Relations


